- Systematic Review
- Open access
- Published:
Prevalence of human papillomavirus in head and neck cancer patients in India: a systematic review and meta-analysis
BMC Infectious Diseases volume 24, Article number: 516 (2024)
Abstract
Background
Human papillomavirus (HPV) is increasingly recognized as a significant risk factor in the development of head and neck cancers (HNCs), with varying prevalence and impact. This study aims to systematically review and analyze the prevalence of HPV in HNCs in India, providing insights into regional variations.
Methods
A comprehensive literature search was carried out using PubMed, Embase, and Web of Science up to November 10, 2023. Inclusion criteria focused on original research reporting HPV-positive cases among HNC patients in India. We used Nested-Knowledge software, for screening, and data extraction. The modified Newcastle-Ottawa Scale was used for quality assessment of included studies. We pooled the prevalence of HPV among HNC patients and performed a random-effects model meta-analysis using R software (version 4.3).
Results
The search yielded 33 studies, encompassing 4654 HNC patients. The pooled prevalence of HPV infection was found to be 33% (95% CI: 25.8–42.6), with notable heterogeneity (I² = 95%). Analysis of subgroups according to geographical location indicated varying prevalence rates. Specifically, the prevalence was 47% (95% CI: 32.2–62.4) in the eastern regions and 19.8% (95% CI: 10.8–33.4) in the western regions. No evidence of publication bias was detected.
Conclusion
The observed considerable regional disparities on the prevalence of HPV in HNC patients in India emphasizes the need for integrated HPV vaccination and screening programs in public health strategies. The findings underline the necessity for further research to explore regional variations and treatment responses in HPV-associated HNCs, considering the impact of factors such as tobacco use and the potential benefits of HPV vaccination.
Introduction
Head and neck cancers (HNC), also known as head and neck squamous cell carcinomas (HNSCC), consist of various malignancies impacting the mucosal surfaces of the upper aerodigestive tract, in areas like the nasopharynx, oral cavity, larynx, oropharynx, hypopharynx, and paranasal sinuses [1]. Annually, HNSCC is responsible for over 650,000 new cancer cases and causes more than 350,000 deaths worldwide [2,3,4]. Traditional primary risk factors for these cancers have been alcohol and tobacco use. However, in recent years, the human papillomavirus (HPV) has been recognized as a significant emerging risk factor, particularly for oropharyngeal squamous cell carcinoma (OPSCC). This has led to the identification of a distinct subtype of HPV-related tumors, which differ from those not associated with HPV. The prevalence of HNSCC tends to vary based on the specific anatomical location and the geographic area [5].
The carcinogenic nature of HPV was definitively established in 1983 when Durst et al. successfully cloned HPV type 16 from cervical carcinoma tissue [6]. It is now widely acknowledged that high-risk HPV types are accountable for almost all cases of cervical cancer. While most HPV infections are asymptomatic and tend to resolve spontaneously, persistent HPV infection in the basal cells of the cervix can lead to the development of cervical cancer [6, 7].
Numerous research articles indicate that epithelial cells from the oral cavity and tonsils can undergo immortalization through the influence of the full-length HPV-16 or its E6/E7 oncogenes [8,9,10,11,12]. Furthermore, studies using transgenic mice have shown that the E6/E7 genes of HPV 16 significantly heighten the risk of developing oral and oropharyngeal cancers [13]. It was found that the E7 gene, in particular, is more effective in triggering these cancers, yet there is a noticeable synergistic effect between E6 and E7 in the genesis of HNSCC [14].
In 2020, India accounted for 7% of the total cancer cases worldwide and a significant 24% of the global incidence of HPV-related cancers [15]. Additionally, it was reported that 80% of cervical cancer cases in India were attributed to HPV subtypes 16 and 18 [16, 17]. As part of its cancer control strategy, India has started implementing opportunistic screening programs for common cancers, including those of the cervix and oral cavity, in its healthcare facilities [18]. A notable increase in HNC occurrences was observed in the population-based cancer registries (PBCRs) for cities such as Aurangabad, Delhi, Chennai, and Bhopal among men, and in Nagpur among women, in India [19]. The age-adjusted incidence rate of HNC stood at approximately 25.9 (95% CI 25.7–26.1) and 8.0 (95% CI 7.9–8.1) per 100,000 people for men and women, respectively [20]. HNC represented around 26% of all cancer diagnoses in men and 8% in women. The likelihood of being diagnosed with HNC was 1 in 33 for men and 1 in 107 for women [20].
Despite the growing body of literature on HPV’s role in HNC, there remains a lack of consensus on its prevalence and impact. This variability is partly due to differences in study designs, population demographics, and detection methods used across various research studies. A systematic review and meta-analysis of the existing studies can provide a more comprehensive understanding of HPV’s prevalence in HNC, offering insights into regional variations.
Method
This systematic review was conducted in accordance with PRISMA guidelines [21] (Table S1) and has been registered in PROSPERO.
Literature search
An electronic literature search was conducted in various databases, including PubMed, Embase, and Web of Science from inception up to November 10, 2023. Keywords and MeSH terms related to HPV and HNC were used to devise the search strategy. No restrictions have been placed on the type of article, year of publication, or language in the search. Table S2 shows the detailed search strategy.
Inclusion criteria
Original research that reports the number of HPV-positive cases among HNC patients is included in this study. We are considering only studies conducted in India. Excluded from this study are case reports, case series, or studies lacking quantitative data. The same exclusion criteria apply to animal studies, commentaries, in vitro studies, and reviews. Studies from any location within India, whether conducted in a hospital or community setting, are eligible. There are no restrictions on the type of test used to detect HPV. A detailed inclusion criterion is specified in Table S3.
Screening and study selection
Two independent reviewers performed the screening of the articles. Nested-Knowledge software was employed for this process. The screening involved a primary review of titles and abstracts, followed by a full-text reading to assess the eligibility of studies for inclusion. An independent third reviewer was consulted to resolve any discrepancies.
Data extraction and quality assessment
Data extraction was performed using the Tag function of the Nested-Knowledge software. Three reviewers carried out the data extraction process. A fourth reviewer cross-checked and validated the extracted data. The data extracted covered the author’s name, year of publication, state/location of the study, study design, age and percentage of males in the sample, total number of HNC patients in the study, number of HPV-positive samples, and the type of test employed for detecting HPV. Quality assessment was done using a modified Newcastle-Ottawa Scale (NOS) version [22, 23].
Statistical analysis
A pooled prevalence of HPV is determined by performing a meta-analysis. A random-effects model is employed to conduct the meta-analysis. The variability in study outcomes was measured using the I2 statistic, which quantifies heterogeneity on a scale from 0 to 100%, where higher values indicate greater heterogeneity [24]. The heterogeneity was further assessed using the 95% prediction interval. We calculated the tau-squared value using maximum likelihood estimation to gain additional insights into heterogeneity [25,26,27,28]. Subgroup analysis was conducted based on the location of the study. We used a funnel plot and the Egger test to detect any potential publication bias. A p-value below 0.05 was typically regarded as statistically significant. All statistical analyses were performed using R software, version 4.3 [23, 29, 30].
Results
Literature search
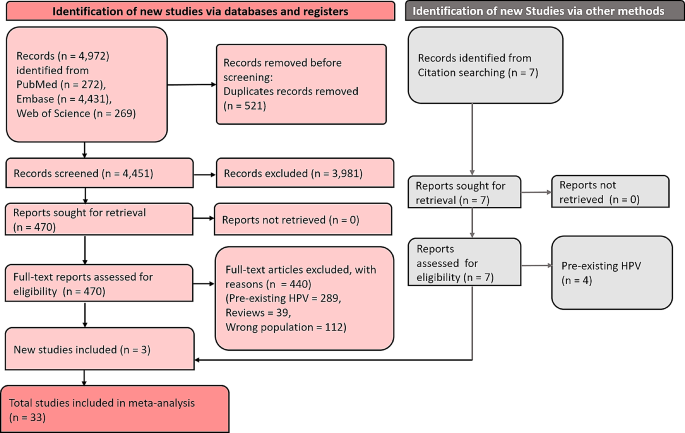
In the literature search, 4,972 articles were identified from multiple databases. Among these, 521 were duplicates. After removing duplicates, 4,451 articles were subjected to screening, of which 3,981 were excluded. The remaining 470 articles were screened by full text for eligibility, resulting in the exclusion of 440, leaving 30 for inclusion. Additionally, 3 studies were added from a citation search. Finally, 33 studies were included in the review. Figure 1 depicts the PRISMA flow chart of the selection and screening process.
Characteristics of included studies
The studies included in this review examining the prevalence of HPV in HNC cases in India are characterized by a diverse methodology and geographical spread. Table 1 summarises the characteristics of included studies. These investigations employ various study designs, including prospective, retrospective, case-control, cohort, and cross-sectional studies, providing a thorough exploration of the subject. The studies are conducted across multiple states and regions of India, representing a broad geographic distribution, and include participants across different age groups, offering insights into age-related variations in HPV prevalence. The proportion of male participants in these studies varies, suggesting potential gender differences in HPV prevalence. The primary diagnostic methods used in these studies are Polymerase Chain Reaction (PCR), genotyping, PCR and P16 Immunohistochemistry (IHC), and Chromogenic In Situ Hybridization (ISH), noted for their high sensitivity. The size of the study populations ranges from small cohorts to large groups, affecting the statistical power of the findings. Rates of HPV positivity exhibit considerable variability, underlining the complexity of understanding HPV prevalence in HNC in this context. These studies span a wide time frame, allowing for the analysis of temporal trends in HPV prevalence. New Delhi contributed 4 studies to the research on HPV prevalence in HNC [31,32,33], while Uttar Pradesh was represented by 5 studies [34,35,36,37,38]. Maharashtra was the focus of 4 studies [39,40,41,42]. Multiple studies were conducted in South India [43, 44], Haryana [45,46,47], and Tamil Nadu [48, 49]. Single studies were conducted in several other locations: Andhra Pradesh [50], Kerala [51], Kolkata [52], Mumbai [53, 54], Karnataka [55, 56], Chandigarh [57, 58], and Assam [59, 60]. Additionally, one study was a multi-regional study encompassing several states [42]. The included studies were overall of moderate to high quality in modified NOS (Table S4).
Meta-analysis
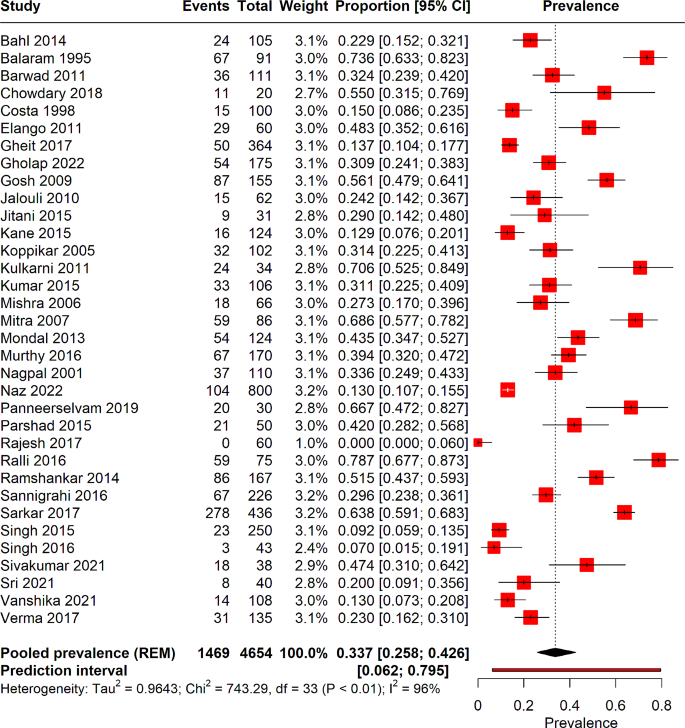
From 33 studies encompassing a total of 4654 patients with HNC, the pooled prevalence of HPV infection was determined to be 33% (95% CI: 25–42%). Notably, substantial heterogeneity was observed among these studies (I² = 96%). A prediction interval ranging from 6.2 to 79% was also observed. Figure 2 illustrates the forest plot depicting the pooled prevalence.
Subgroup analysis
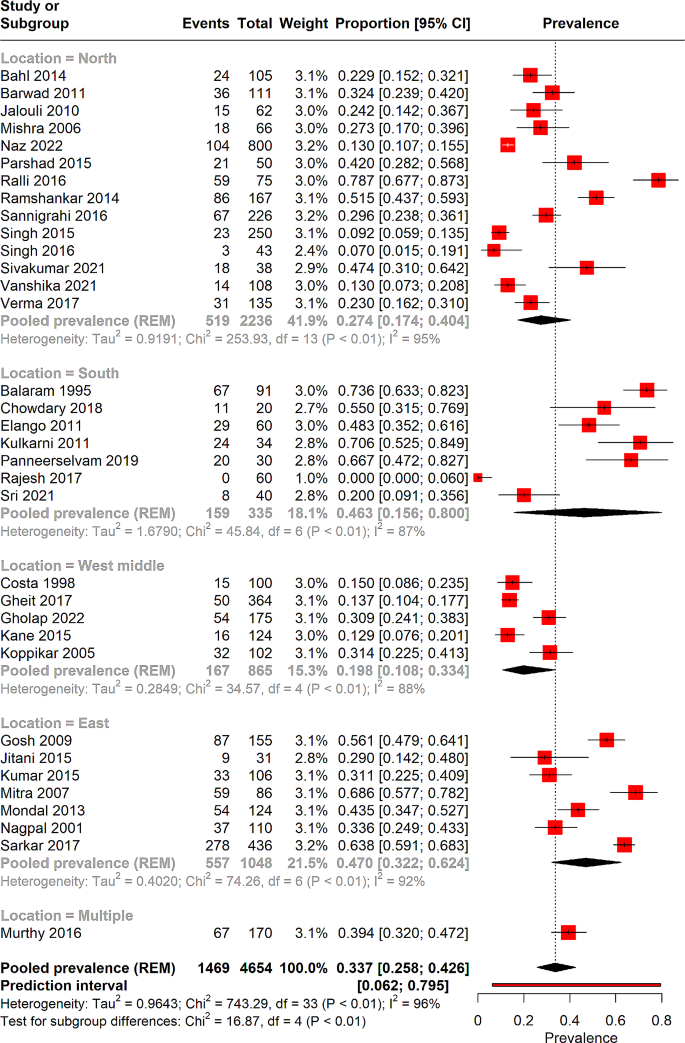
Subgroup analysis was performed on the basis of the location of the study (Fig. 3). The North region is represented by 14 studies encompassing a total of 2236 patients, revealing a pooled HPV prevalence of 27% (95% CI: 17.4–40.4%), and a high degree of heterogeneity (I² = 95%). The South region, with 7 studies and 335 patients, has a pooled prevalence of 46.3% (95% CI: 15.6–80%), also accompanied by significant heterogeneity (I² = 87%). In the West Middle region, 5 studies totalling 865 patients show a pooled prevalence of 19.8% (95% CI: 10.8–33.4%) with substantial heterogeneity (I² = 88%). A single study spans multiple locations—Madhya Pradesh, Gujarat, Rajasthan, Uttar Pradesh, West Bengal, and Assam—encompassing 170 patients and reporting a higher pooled prevalence of 39% (95% CI: 32–47%). Lastly, the East region, represented by 7 studies with 1048 patients, presents a pooled prevalence of 47% (95% CI: 32.2–62.4%) with high heterogeneity (I² = 92%).
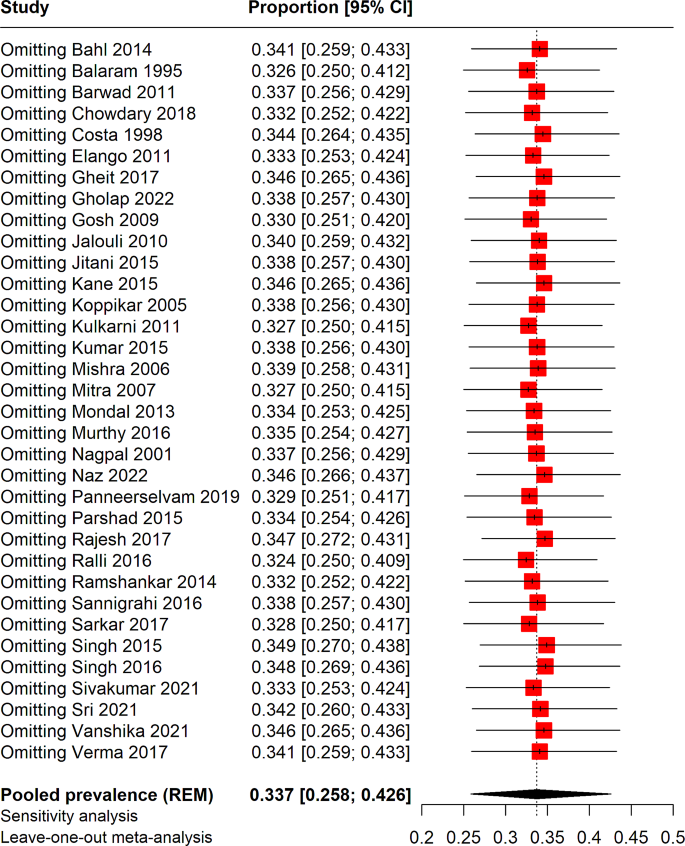
Meta-regression and sensitivity analysis
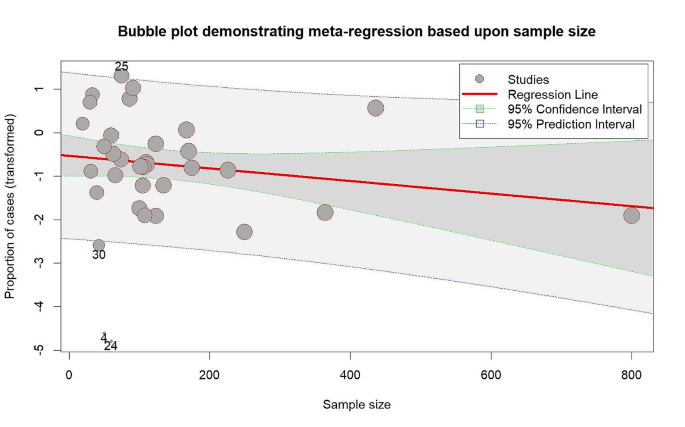
Meta-regression was performed to determine the effect of sample size on the pooled prevalence of HPV in HNC cases, as depicted in Fig. 4. However, the meta-regression analysis indicated that sample size was not significantly associated with the pooled prevalence results (p = 0.20). Additionally, a leave-one-out sensitivity analysis was conducted to identify individual studies that might affect the overall prevalence rate. This analysis revealed that the exclusion of no single study resulted in any significant changes to the overall pooled prevalence, as illustrated in Fig. 5.
Publication bias
Publication bias was assessed using funnel plot asymmetry and Egger’s test, as shown in Figure S1. The results of our analysis did not provide evidence of publication bias (Egger’s test, p = 0.71).
Discussion
In the best of our knowledge, this is the first meta-analysis to determine the prevalence of HPV among HNC patients in India. In our analysis, we found an overall prevalence of 33% for HPV among HNC patients. South India and the eastern part of India have shown slightly greater prevalence compared to the north and west parts of India. Meta-regression, sensitivity analysis couldn’t resolve the s0000ource of heterogeneity.
Previous systematic reviews have established evidence that infection with HPV is a distinct risk factor for developing HNCs [61, 62]. The risk associated with tonsil carcinoma is notably high and aligns with what one would anticipate from an infectious cause. Our findings indicate that HPV’s involvement in tonsil cancer is similar to the role of Epstein-Barr virus in nasopharyngeal cancer, suggesting that this is yet another instance of a virus-induced cancer in the pharyngeal lymphoid tissue [62].
The risk associated with the progression or death, along with the likelihood of developing a secondary primary HNOSCC, increases by 1% and 1.5% respectively for each additional year of smoking. This remains true even when accounting for the HPV tumor status and other important factors. Importantly, the risk of death doubles for patients who continue smoking during radiation therapy. The detection of HPV in HNCs is highly significant for prognosis and can influence the modification of treatment plans based on the HPV status [63]. Thus, the accurate identification of HPV as a contributing factor in HNCs is of paramount importance. Typically, a biopsy or cytological analysis from the primary tumor site or enlarged lymph nodes is crucial for an initial diagnosis. PCR or RT-PCR (Reverse Transcriptase-PCR) are commonly employed methods for detecting HPV in tumor tissues, particularly for identifying E6/E7 in fresh frozen samples. However, these methods are associated with high setup costs and longer turnaround times [64].
The presence of HPV in HNCs significantly alters the disease’s prognosis and therapeutic approach. HPV-positive HNCs typically present with a better response to standard treatment modalities like radiotherapy and chemotherapy, leading to an overall better prognosis compared to HPV-negative cases [65]. This is primarily attributed to the distinct biological behavior of HPV-positive tumors, which tend to be more sensitive to radiation and cytotoxic agents. Studies has indicated that individuals diagnosed with HPV-positive oropharyngeal cancer have higher survival rates and lower risks of recurrence [66].
Given these differences, there is an emerging consensus on tailoring treatment strategies based on HPV status. For instance, the concept of treatment de-escalation for HPV-positive HNCs is gaining traction. This approach involves reducing the intensity of standard treatments to minimize long-term side effects without compromising the efficacy of cancer control [67]. Clinical trials are currently exploring various de-escalation strategies, including reduced-dose radiotherapy, omission of chemotherapy, and the use of minimally invasive surgeries [68, 69]. However, it’s important to approach de-escalation cautiously, ensuring that patient selection is based on robust biomarkers and clinical criteria to avoid under-treatment.
The accurate determination of HPV status in HNCs is pivotal for both prognostic assessment and guiding treatment decisions. Polymerase Chain Reaction (PCR) and Reverse Transcriptase-PCR (RT-PCR) are the gold standards for detecting HPV, particularly E6/E7 mRNA, in tumor tissues [70,71,72]. These methods are highly sensitive and specific but are often hindered by high costs and longer turnaround times, posing challenges in resource-limited settings. Emerging diagnostic techniques, such as liquid biopsies and next-generation sequencing (NGS), are promising alternatives. Liquid biopsies, which detect circulating tumor DNA (ctDNA) in blood samples, offer a less invasive method for HPV detection and monitoring [73,74,75]. NGS, on the other hand, allows for the comprehensive analysis of HPV integration sites and co-mutations, providing a more detailed tumor profile [76]. These technologies not only improve the accessibility of HPV testing but also enhance our understanding of the tumor biology, which is crucial for personalized medicine.
The significant role of HPV in HNCs necessitates public health interventions, particularly in countries like India where the burden of these cancers is high. HPV vaccination, which has been successful in reducing the incidence of cervical cancer, presents a viable strategy to curb HPV-related HNCs. The expansion of HPV vaccination programs to include both girls and boys could significantly reduce the future burden of these cancers [77, 78]. It is crucial to integrate HPV vaccination into national immunization programs and to raise public awareness about its benefits. Furthermore, the compounded risk of tobacco use in HPV-positive HNC patients highlights the urgent need for effective tobacco cessation programs. Tobacco, being a well-established risk factor for HNCs, exacerbates the risk even in the context of HPV-positive cancers. Public health campaigns targeting tobacco cessation are not only essential for preventing HNCs but also for improving outcomes in patients with existing HPV-related cancers [79,80,81].
Our study acknowledges certain limitations that should be considered. Firstly, our analysis was restricted to articles published in the English language, potentially omitting relevant research published in other languages. Additionally, the geographic coverage of our data is not comprehensive; studies from all regions of India were not available, which may affect the generalizability of our findings. While subgroup analysis was conducted, it was not sufficient to completely address the sources of heterogeneity observed in the results. We were unable to perform subgroup analysis based on site-specific cancer prevalence due to the unavailability of reported data. Future studies should include detailed data on site-specific HNC and HPV to facilitate more comprehensive analyses. This heterogeneity could stem from various factors such as differences in study design, populations, or methodologies, which our subgroup analysis could not fully disentangle. The overall sample size of the included studies was relatively small. This limitation could impact the statistical power of our findings and might lead to less precise estimates. Given these constraints, we recommend that future research should include a broader range of languages and geographic areas, especially underrepresented regions of India. More extensive studies with larger sample sizes would also be beneficial to provide more robust and generalizable results, and to further explore the sources of heterogeneity observed in this study. The absence of publication bias in our findings further strengthens the reliability of these insights.
Conclusion
This comprehensive study underscores the significant role of HPV in the epidemiology of HNCs in India. Through a detailed systematic review and meta-analysis, we determined that the pooled prevalence of HPV among HNC patients in India is 33%, revealing a substantial impact of this virus on such cancers. Notably, the study highlighted regional variations, with the highest prevalence in eastern India (47%) and lowest in the western regions (∼ 20%). This variability suggests the influence of regional factors in the prevalence and impact of HPV in HNCs. Overall, our study provides valuable data for healthcare professionals and policymakers, emphasizing the need for targeted interventions and policies to address the HPV-related burden in HNC patients in India, while also considering the regional disparities in prevalence and risk factors.
Data availability
All the data used in this review has been provided in the manuscript and supplementary files.
References
Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR. Head and neck squamous cell carcinoma. Nat Reviews Disease Primers. 2020;6(1):92.
Leemans CR, Snijders PJ, Brakenhoff RH. The molecular landscape of head and neck cancer. Nat Rev Cancer. 2018;18(5):269–82.
Hashim D, Genden E, Posner M, Hashibe M, Boffetta P. Head and neck cancer prevention: from primary prevention to impact of clinicians on reducing burden. Ann Oncol. 2019;30(5):744–56.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68(6):394–424.
Sabatini ME, Chiocca S. Human papillomavirus as a driver of head and neck cancers. Br J Cancer. 2020;122(3):306–14.
Dürst M, Gissmann L, Ikenberg H, Zur Hausen H. A papillomavirus DNA from a cervical carcinoma and its prevalence in cancer biopsy samples from different geographic regions. Proc Natl Acad Sci. 1983;80(12):3812–5.
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–9.
Lace MJ, Anson JR, Klussmann JP, Wang DH, Smith EM, Haugen TH, et al. Human papillomavirus type 16 (HPV-16) genomes integrated in head and neck cancers and in HPV-16-immortalized human keratinocyte clones express chimeric virus-cell mRNAs similar to those found in cervical cancers. J Virol. 2011;85(4):1645–54.
Sexton CJ, Proby CM, Banks La, Stables JN, Powell K, Navsaria H, et al. Characterization of factors involved in human papillomavirus type 16-mediated immortalization of oral keratinocytes. J Gen Virol. 1993;74(4):755–61.
Smeets SJ, van der Plas M, Schaaij-Visser TB, van Veen EA, van Meerloo J, Braakhuis BJ, et al. Immortalization of oral keratinocytes by functional inactivation of the p53 and pRb pathways. Int J Cancer. 2011;128(7):1596–605.
Park N-H, Min B-M, Li S-l, Huang MZ, Doniger J. Immortalization of normal human oral keratinocytes with type 16 human papillomavirus. Carcinogenesis. 1991;12(9):1627–31.
Chen R, Aalto Y, Teesalu T, Dürst M, Knuutila S, Aaltonen L-M, et al. Establishment and characterisation of human papillomavirus type 16 DNA immortalised human tonsillar epithelial cell lines. Eur J Cancer. 2003;39(5):698–707.
Strati K, Pitot HC, Lambert PF. Identification of biomarkers that distinguish human papillomavirus (HPV)-positive versus HPV-negative head and neck cancers in a mouse model. Proc Natl Acad Sci. 2006;103(38):14152–7.
Jabbar S, Strati K, Shin MK, Pitot HC, Lambert PF. Human papillomavirus type 16 E6 and E7 oncoproteins act synergistically to cause head and neck cancer in mice. Virology. 2010;407(1):60–7.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021;71(3):209–49.
Basu P, Roychowdhury S, Bafna UD, Chaudhury S, Kothari S, Sekhon R, et al. Human papillomavirus genotype distribution in cervical cancer in India: results from a multi-center study. Asian Pac J Cancer Prev. 2009;10(1):27–34.
Senapati R, Nayak B, Kar SK, Dwibedi B. HPV genotypes distribution in Indian women with and without cervical carcinoma: implication for HPV vaccination program in Odisha, Eastern India. BMC Infect Dis. 2017;17:1–10.
Lohiya A, Daniel RA, Smith RD, Nagar M, Shankar A, Lahariya C. Cancer prevention and control in India can get a boost through primary health care-based approach: a review. J Family Med Prim Care. 2022;11(8):4286.
ICMR National Centre for Disease Informatics and Research: National Cancer Registry Programme Report Bengaluru, India. 2020 [ https://ncdirindia.org/All_Reports/PBCR_Annexures/Default.aspx.
Bagal S, Budukh A, Thakur JS, Dora T, Qayyumi B, Khanna D et al. Head and neck cancer burden in India: an analysis from published data of 37 population-based cancer registries. Ecancermedicalscience. 2023;17.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Bushi G, Shabil M, Padhi BK, Ahmed M, Pandey P, Satapathy P, et al. Prevalence of acute kidney injury among dengue cases: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 2023;118(1):1–11.
Bushi G, Padhi BK, Shabil M, Satapathy P, Rustagi S, Pradhan KB, et al. Cardiovascular Disease outcomes Associated with Obstructive Sleep Apnea in diabetics: a systematic review and Meta-analysis. Diseases. 2023;11(3):103.
Gandhi AP, Satapathy P, Rustagi S, Hermis AH, Sah R, Padhi BK. Comments on shigellosis in Southeast Asia: a systematic review and meta-analysis. Travel Med Infect Dis. 2023:102593-.
Langan D, Higgins JP, Jackson D, Bowden J, Veroniki AA, Kontopantelis E, et al. A comparison of heterogeneity variance estimators in simulated random-effects meta‐analyses. Res Synthesis Methods. 2019;10(1):83–98.
Gandhi AP, Shamim MA, Padhi BK. Steps in undertaking meta-analysis and addressing heterogeneity in meta-analysis. Evid. 2023;1(1):44–59.
Shabil M, Bushi G, Beig MA, Rais MA, Ahmed M, Padhi BK. Cardiovascular manifestation in tuberculosis cases: a systematic review and Meta-analysis. Curr Probl Cardiol. 2023;48(7):101666.
Bushi G, Shabil M, Padhi BK, Ahmed M, Pandey P, Satapathy P, et al. Prevalence of acute kidney injury among dengue cases: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 2024;118(1):1–11.
Alrahbeni T, Mahal A, Alkhouri A, Alotaibi HF, Rajagopal V, Behera A et al. Surgical interventions for intractable migraine: a systematic review and meta-analysis. International Journal of Surgery.10.1097.
Swarup SS, Padhi BK, Satapathy P, Shabil M, Bushi G, Gandhi AP et al. Cardiovascular consequences of financial stress: a systematic review and meta-analysis. Curr Probl Cardiol. 2023:102153.
Bahl A, Kumar P, Dar L, Mohanti BK, Sharma A, Thakar A, et al. Prevalence and trends of human papillomavirus in oropharyngeal cancer in a predominantly north Indian population. Head Neck. 2014;36(4):505–10.
Mishra A, Bharti AC, Varghese P, Saluja D, Das BC. Differential expression and activation of NF-κB family proteins during oral carcinogenesis: role of high risk human papillomavirus infection. Int J Cancer. 2006;119(12):2840–50.
Naz F, Verma H, Tanveer N, Sudheer AK, Kakkar A, Tanwar P. Demographic Profile of p16 immunopositive and HPV DNA PCR positive oral squamous cell carcinoma in a large cohort of Indian patients. Asian Pac J Cancer Prevention: APJCP. 2022;23(2):529.
Jalouli J, Ibrahim SO, Mehrotra R, Jalouli MM, Sapkota D, Larsson P-A, et al. Prevalence of viral (HPV, EBV, HSV) infections in oral submucous fibrosis and oral cancer from India. Acta Otolaryngol. 2010;130(11):1306–11.
Singh V, Husain N, Akhtar N, Kumar V, Tewari S, Mishra S, et al. Do human papilloma viruses play any role in oral squamous cell carcinoma in North indians? Asian Pac J Cancer Prev. 2015;16(16):7077–84.
Singh AK, Kushwaha JK, Anand A, Sonkar AA, Husain N, Srivastava K, et al. Human papilloma virus in oral cavity cancer and relation to change in quality of life following treatment—A pilot study from Northern India. Indian J Surg Oncol. 2016;7:386–91.
Vanshika S, Preeti A, Sumaira Q, Vijay K, Shikha T, Shivanjali R, et al. Incidence OF HPV and EBV in oral cancer and their clinico-pathological correlation–a pilot study of 108 cases. J Oral Biology Craniofac Res. 2021;11(2):180–4.
Verma G, Vishnoi K, Tyagi A, Jadli M, Singh T, Goel A, et al. Characterization of key transcription factors as molecular signatures of HPV-positive and HPV‐negative oral cancers. Cancer Med. 2017;6(3):591–604.
Gheit T, Anantharaman D, Holzinger D, Alemany L, Tous S, Lucas E, et al. Role of mucosal high-risk human papillomavirus types in head and neck cancers in central India. Int J Cancer. 2017;141(1):143–51.
Gholap D, Mhatre S, Chaturvedi P, Nair S, Gheit T, Tommasino M et al. Prevalence of human papillomavirus types in head and neck cancer sub-sites in the Indian population. Ecancermedicalscience. 2022;16.
Kane S, Patil V, Noronha V, Joshi A, Dhumal S, D’Cruz A, et al. Predictivity of human papillomavirus positivity in advanced oral cancer. Indian J câncer. 2015;52(3):403–5.
Murthy V, Swain M, Teni T, Pawar S, Kalkar P, Patil A, et al. Human papillomavirus/p16 positive head and neck cancer in India: prevalence, clinical impact, and influence of tobacco use. Indian J Cancer. 2016;53(3):387–93.
Elango KJ, Suresh A, Subhadradevi L, Ravindran HK, Iyer SK, Iyer S, et al. Role of human papilloma virus in oral tongue squamous cell carcinoma. Asian Pac J Cancer Prev. 2011;12(4):889–96.
Panneerselvam K, Rameshkumar A, Rajkumar K, Ramadoss R. Detection of human papillomavirus 16 and 18 in patients with oral squamous cell carcinoma and potentially malignant oral disorders in South Indian population: a pilot study. J Cancer Res Ther. 2019;15(3):571–5.
Parshad S, Nandi S, Marwah N, Mehta P, Tripathi M, Gogna S, et al. Human papillomavirus 16 and 18 in squamous cell carcinoma of oral cavity and sexual practices: a pilot study at a Tertiary Care Hospital of North India. Natl J Maxillofacial Surg. 2015;6(2):185.
Ralli M, Singh S, Yadav S, Sharma N, Verma R, Sen R. Assessment and clinicopathological correlation of p16 expression in head and neck squamous cell carcinoma. J Cancer Res Ther. 2016;12(1):232–7.
Sivakumar N, Narwal A, Kamboj M, Devi A, Kumar S, Bhardwaj R. Molecular and immunohistochemical cognizance of HPV16 in oral leukoplakia, oral squamous cell carcinoma and oropharyngeal squamous cell carcinoma. Head Neck Pathol. 2021;15:882–92.
Ramshankar V, Soundara VT, Shyamsundar V, Ramani P, Krishnamurthy A. Risk stratification of early stage oral tongue cancers based on HPV status and p16 immunoexpression. Asian Pac J Cancer Prev. 2014;15(19):8351–9.
Sri S, Ramani P, Premkumar P, Ramshankar V, Ramasubramanian A, Krishnan RP. Prevalence of human papillomavirus (HPV) 16 and 18 in oral malignant and potentially malignant disorders: a polymerase chain reaction analysis–A comparative study. Annals Maxillofacial Surg. 2021;11(1):6.
Chowdary SD, Sekhar PC, Kattapagari KK, Deepthi CM, Neelima D, Reddy BVR. A study to assess expression of human papillomavirus types 16 and 18 in oral squamous cell carcinoma using polymerase chain reaction. J Oral Maxillofacial Pathology: JOMFP. 2018;22(3):347.
Balaram P, Nalinakumari KR, Abraham E, Balan A, Hareendran NK, Bernard HU, et al. Human papillomaviruses in 91 oral cancers from Indian betel quid chewers–high prevalence and multiplicity of infections. Int J Cancer. 1995;61(4):450–4.
Jitani AK, Raphael V, Mishra J, Shunyu NB, Khonglah Y, Medhi J. Analysis of human papilloma virus 16/18 DNA and its correlation with p16 expression in oral cavity squamous cell carcinoma in North-Eastern India: a chromogenic in-situ hybridization based study. J Clin Diagn Research: JCDR. 2015;9(8):EC04.
D’Costa J, Saranath D, Dedhia P, Sanghvi V, Mehta AR. Detection of HPV-16 genome in human oral cancers and potentially malignant lesions from India. Oral Oncol. 1998;34(5):413–20.
Koppikar P, deVilliers EM, Mulherkar R. Identification of human papillomaviruses in tumors of the oral cavity in an Indian community. Int J Cancer. 2005;113(6):946–50.
Kulkarni SS, Kulkarni SS, Vastrad PP, Kulkarni BB, Markande AR, Kadakol G, et al. Prevalence and distribution of high risk human papillomavirus (HPV) types 16 and 18 in Carcinoma of cervix, saliva of patients with oral squamous cell carcinoma and in the general population in Karnataka, India. Asian Pac J Cancer Prev. 2011;12(3):645–8.
Rajesh D, Mohiyuddin SA, Kutty AM, Balakrishna S. Prevalence of human papillomavirus in oral squamous cell carcinoma: a rural teaching hospital-based cross-sectional study. Indian J Cancer. 2017;54(3):498–501.
Barwad A, Sood S, Gupta N, Rajwanshi A, Panda N, Srinivasan R. Human papilloma virus associated head and neck cancer: a PCR based study. Diagn Cytopathol. 2012;40(10):893–7.
Sannigrahi M, Singh V, Sharma R, Panda N, Radotra B, Khullar M. Detection of active human papilloma virus-16 in head and neck cancers of Asian north Indian patients. Oral Dis. 2016;22(1):62–8.
Kumar R, Rai AK, Das D, Das R, Kumar RS, Sarma A, et al. Alcohol and tobacco increases risk of high risk HPV infection in head and neck cancer patients: study from North-East Region of India. PLoS ONE. 2015;10(10):e0140700.
Mondal R, Ghosh SK, Choudhury JH, Seram A, Sinha K, Hussain M, et al. Mitochondrial DNA copy number and risk of oral cancer: a report from Northeast India. PLoS ONE. 2013;8(3):e57771.
Pinkiewicz M, Dorobisz K, Zatoński T. Human Papillomavirus-Associated Head and Neck Cancers. Where are we now? A systematic review. Cancer Manage Res. 2022:3313–24.
Hobbs C, Sterne J, Bailey M, Heyderman R, Birchall M, Thomas S. Human papillomavirus and head and neck cancer: a systematic review and meta-analysis. Clin Otolaryngol. 2006;31(4):259–66.
Gillison ML, Zhang Q, Jordan R, Xiao W, Westra WH, Trotti A, et al. Tobacco smoking and increased risk of death and progression for patients with p16-positive and p16-negative oropharyngeal cancer. J Clin Oncol. 2012;30(17):2102.
Würdemann N, Wagner S, Sharma SJ, Prigge E-S, Reuschenbach M, Gattenlöhner S, et al. Prognostic impact of AJCC/UICC 8th edition new staging rules in oropharyngeal squamous cell carcinoma. Front Oncol. 2017;7:129.
Saba NF, Pamulapati S, Patel B, Mody M, Strojan P, Takes R, et al. Novel immunotherapeutic approaches to treating HPV-Related Head and Neck Cancer. Cancers. 2023;15(7):1959.
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24–35.
Economopoulou P, Kotsantis I, Psyrri A. De-escalating strategies in HPV-associated head and neck squamous cell carcinoma. Viruses. 2021;13(9):1787.
Mirghani H, Blanchard P. Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Translational Radiation Oncol. 2018;8:4–11.
Mensour EA, Alam S, Mawani S, Bahig H, Lang P, Nichols A, et al. What is the future of treatment de-escalation for HPV-positive oropharyngeal cancer? A review of ongoing clinical trials. Front Oncol. 2022;12:1067321.
Sun Y, Wang Z, Qiu S, Wang R. Therapeutic strategies of different HPV status in head and neck squamous cell carcinoma. Int J Biol Sci. 2021;17(4):1104.
Eggersmann TK, Baumeister P, Kumbrink J, Mayr D, Schmoeckel E, Thaler CJ, et al. Oropharyngeal HPV detection techniques in HPV-associated head and neck cancer patients. Anticancer Res. 2020;40(4):2117–23.
Shabil M, Murti K, Kumar VU, Kumar R, Kumar N, Dhingra S, et al. Older PLHIV are at Higher Cardiovascular Risk with Poor Quality of Life. Curr HIV Res. 2023;21(6):354–60.
Rostami A, Bratman SV, Han K. Liquid Biopsy goes viral: next-generation sequencing to enhance HPV detection. Clin Cancer Res. 2021;27(19):5158–60.
Faden DL. Liquid biopsy for the diagnosis of HPV-associated head and neck cancer. Cancer Cytopathol. 2022;130(1):12–5.
Goel S, Shabil M, Kaur J, Chauhan A, Rinkoo AV. Safety, efficacy and health impact of electronic nicotine delivery systems (ENDS): an umbrella review protocol. BMJ open. 2024;14(1):e080274.
Zhou L, Qiu Q, Zhou Q, Li J, Yu M, Li K, et al. Long-read sequencing unveils high-resolution HPV integration and its oncogenic progression in cervical cancer. Nat Commun. 2022;13(1):2563.
Qendri V, Bogaards JA, Berkhof J. Who will benefit from expanding HPV vaccination programs to boys? JNCI cancer spectrum. 2018;2(4):pky076.
Pearson AL, Kvizhinadze G, Wilson N, Smith M, Canfell K, Blakely T. Is expanding HPV vaccination programs to include school-aged boys likely to be value-for-money: a cost-utility analysis in a country with an existing school-girl program. BMC Infect Dis. 2014;14(1):1–15.
Hoover DS, Spears CA, Vidrine DJ, Walker JL, Shih Y-CT, Wetter DW. Smoking cessation treatment needs of low SES cervical cancer survivors. Am J Health Behav. 2019;43(3):606–20.
Patterson JG, Borger TN, Burris JL, Conaway M, Klesges R, Ashcraft A, et al. A cluster randomized controlled trial for a multi-level, clinic-based smoking cessation program with women in Appalachian communities: study protocol for the Break Free program. Addict Sci Clin Pract. 2022;17(1):1–15.
Shabil M, Kumar VU, Dhingra S, Ravichandiran V, Parihar VK, Kumar N, et al. Current scenario and strategies to Tackle Cardiovascular Disease Risk in HIV Geriatrics. Curr Pharmacol Rep. 2023;9(6):523–39.
Mitra S, Banerjee S, Misra C, Singh RK, Roy A, Sengupta A, et al. Interplay between human papilloma virus infection and p53 gene alterations in head and neck squamous cell carcinoma of an Indian patient population. J Clin Pathol. 2007;60(9):1040–7.
Nagpal JK, Patnaik S, Das BR. Prevalence of high-risk human papilloma virus types and its association with P53 codon 72 polymorphism in tobacco addicted oral squamous cell carcinoma (OSCC) patients of Eastern India. Int J Cancer. 2002;97(5):649–53.
Sarkar S, Alam N, Chakraborty J, Biswas J, Mandal SS, Roychoudhury S, et al. Human papilloma virus (HPV) infection leads to the development of head and neck lesions but offers better prognosis in malignant Indian patients. Med Microbiol Immunol. 2017;206:267–76.
Acknowledgements
The authors acknowledge the Nested-Knowledge, MN, USA for providing the access to the software.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Substantial contribution to the conception or design of the work: PS, HAS, RKS. Acquisition of data: MNK, SG, QSZ, MA. Analysis and interpretation of data for the work: SR, AAR, MFS. Drafting the work: HAA, ASA, PS, MNK, DS, MA. Revising it critically for important intellectual content: AA, HAS, HAR, QSZ, AN, MA. Resources: Q.S.Z, P.S, M.N.K, B.K.P, J.K.G, D.N, MA. Final approval of the version to be published: All authors (PS, MNK, SG, QSZ, HAS, RKS, DS, MA, SR, AN, AA, MA, MFA, MA, MA, AR). Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: All authors (PS, MNK, SG, QSZ, HAS, RKS, DS, MA, SR, AN, AA, MA, MFA, MA, MA, AR).
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
Authors declare no conflicts of interests.
Ethical approval
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Satapathy, P., Khatib, M.N., Gaidhane, S. et al. Prevalence of human papillomavirus in head and neck cancer patients in India: a systematic review and meta-analysis. BMC Infect Dis 24, 516 (2024). https://doi.org/10.1186/s12879-024-09357-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09357-2